Introduction For decades, metal plates, rods, and screws have been the backbone of fracture treatment. While effective, they can require invasive surgery, prolonged recovery, and sometimes a second operation for removal. Enter bone glue—also called surgical bone adhesive—a fast-evolving class of biocompatible materials designed to bond fractured bone segments. This bone healing technology aims to support minimally invasive bone repair, stabilize fractures, and promote natural regeneration without bulky hardware in suitable cases. Recent advances in orthopedic adhesive technology and bone bonding polymer science are bringing bone repair glue closer to real-world surgical use.
In this in-depth guide, we explain how bone adhesives work, where they could help, what limitations remain, and what the research says so far.
Key takeaways (bullet summary)
- Bone glue is a biocompatible bone adhesive that can bond bone surfaces, potentially reducing the need for metal hardware in select fractures.
- Surgical bone adhesive is not for every fracture; load-bearing bones and complex patterns may still need plates or screws.
- The latest bone healing technology uses bone bonding polymers engineered for strength, biocompatibility, and osteointegration.
- Safety, curing speed, imaging compatibility, and long-term durability are the core evaluation metrics in clinical research.
- Early data shows promise for minimally invasive bone repair, pediatric use, and craniofacial or small-fragment fixation.
- Ongoing trials and regulatory review will determine how quickly this bone fracture treatment innovation enters mainstream practice.
What is bone glue? Bone glue refers to a medical adhesive designed specifically for bone tissue. Unlike soft-tissue glues used for skin or organs, a bone adhesive must withstand higher loads, integrate with mineralized tissue, and maintain stability in a moist, blood-rich environment. Modern formulations include:
- (e.g., modified cyanoacrylates, methacrylate resins) tuned for lower toxicity and better flexibility
- Biomimetic bioadhesive for bones that emulate natural bone proteins and mineral phases
- Biocompatible bone glue with osteoconductive fillers (e.g., calcium phosphate) for osteointegration
- Hybrid systems that combine medical adhesive for fractures with reinforcement fibers or meshes
How bone adhesives work At a high level, bone repair glue adheres through a combination of surface wetting, chemical bonding, and micro-mechanical interlocking:
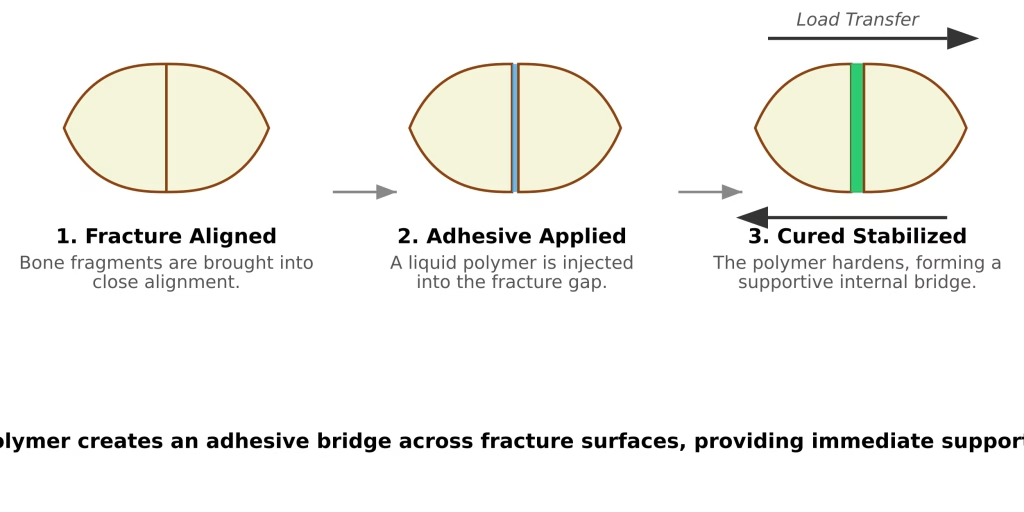
- Surface preparation: Surgeons dry and prepare the fracture interface to maximize contact.
- Application: A surgical bone adhesive is applied as a liquid or paste.
- Curing: The material sets (chemically or via light/dual-cure), forming a rigid or semi-rigid matrix.
- Osteointegration: Some osteointegration adhesives encourage bone cells to colonize the interface, gradually strengthening the bond.
- Remodeling: Ideally, the adhesive either persists safely long-term or resorbs in step with new bone formation, aligning with bone regeneration materials research.
Potential benefits
- Minimally invasive bone repair: smaller incisions, less soft-tissue disruption, and shorter OR time in appropriate cases.
- Precision alignment: The adhesive can hold fine fragments in place, especially in facial, hand, and pediatric fractures.
- Reduced hardware complications: Less metal may mean fewer issues like hardware prominence or cold sensitivity.
- “Instant” support: Some systems provide rapid initial fixation—often described as instant bone fracture repair support—while the body heals.
Where bone glue may fit clinically
- Craniofacial and maxillofacial fractures (e.g., orbital rim, zygomatic arch) with delicate fragments
- Small bone and fragment fixation (hand, foot, patella fragments)
- Pediatric fractures, where growth plates and future bone development are concerns
- Augmenting screws or plates to improve interface bonding in osteoporotic bone
- Targeted applications in minimally invasive bone repair for select non-load-bearing regions
Where caution is needed
- High-load, weight-bearing sites (e.g., femoral shaft) still generally require mechanical fixation.
- Complex, comminuted fractures under torsion or shear may exceed current adhesive strengths.
- Heat generation during curing, local cytotoxicity, and reversibility remain important considerations in product design.
Safety and biocompatibility The safety profile of biocompatible bone glue is central to adoption:
- Cytocompatibility: Low toxicity to osteoblasts and surrounding tissues.
- Thermal control: Exothermic reactions must be moderated to avoid thermal injury.
- Degradation: If degradable, byproducts should be benign and cleared naturally.
- Imaging: Compatibility with X-ray, CT, and MRI—no heavy artifacts that obscure follow-up care.
- Infection resistance: Some formulations integrate antimicrobial agents to reduce infection risks.
- Osteointegration: Osteointegration adhesives aim for a biologically friendly interface that encourages bone ingrowth for longer-term stability.
Performance metrics that matter
- Bond strength and toughness: Ability to withstand physiological loading and micro-motions.
- Curing time and handling: Surgeons need predictable working and setting times.
- Moisture tolerance: Effective adhesion in the wet surgical field.
- Elastic modulus: Sufficient stiffness without becoming too brittle.
- Fatigue resistance: Durability under repeated stresses until bone union.
- Reworkability: Capacity to reposition fragments or remove adhesive if necessary.
Research landscape and leading directions The field of orthopedic adhesive technology is rapidly evolving. Key research themes include:
- Bioinspired designs: Mimicking mussel adhesive proteins (catechols) for strong wet adhesion.
- Mineral-integrating chemistries: Calcium phosphate–reinforced bone bonding polymers that promote osteoconductivity.
- Dual-cure systems: Light plus chemical curing for deeper and faster set.
- 3D-printable pastes: Custom-shaped scaffolds that double as medical adhesive for fractures and bone regeneration materials.
- Smart additives: Radiopacifiers for imaging and antimicrobial nanoparticles to reduce infection.
Clinical evidence is growing, with early-stage trials indicating feasibility for specific indications. However, widespread replacement of plates and screws is unlikely in the short term. Instead, expect bone glue to emerge as a complementary tool—especially in small-fragment fixation, craniofacial applications, and as an adjunct to hardware in osteoporotic bone.
Comparison: surgical bone adhesive vs traditional fixation
- Invasiveness: Adhesives can enable smaller incisions; hardware typically requires larger exposures.
- Immediate stability: High with plates/screws; variable with adhesives depending on formulation and site.
- Hardware prominence: None with adhesives; possible with plates.
- Revision options: Familiar with hardware; adhesives must be designed for removability or safe persistence.
- Cost and availability: Adhesives are emerging; hardware is widely available and standardized.
in a nutshell, by combining biocompatible chemistry with clinical insight, orthopedic adhesive technology may enable more precise, minimally invasive bone repair in selected cases. While it won’t replace plates and screws across the board, this bone healing technology is poised to become a valuable tool for surgeons and a hopeful development for patients seeking faster, less invasive recovery.